HIV Explained: Early Signs, Risk Factors, and Immune Response
Human Immunodeficiency Virus, commonly known as HIV, remains a significant public health concern affecting millions worldwide. Understanding the early indicators of HIV infection, recognizing why symptoms often go unnoticed, and learning how the immune system responds to viral challenges are crucial steps in promoting awareness and encouraging timely medical intervention. This article explores the biological mechanisms behind HIV, the subtle signs that may emerge during initial infection, and the various factors that influence how individuals experience and recognize these symptoms.
HIV is a retrovirus that specifically targets CD4+ T cells, which are essential components of the immune system. When the virus enters the body, it begins replicating rapidly, leading to a cascade of immune responses that can manifest in various ways. The progression from initial infection to potential complications follows a predictable pattern, though individual experiences may vary significantly based on numerous factors including overall health status, age, and access to medical care.
Common Early Signs That May Appear
The acute phase of HIV infection, typically occurring 2-4 weeks after exposure, often presents with flu-like symptoms that can easily be mistaken for common illnesses. Fever is among the most frequent early indicators, often accompanied by fatigue that seems disproportionate to typical tiredness. Many individuals experience swollen lymph nodes, particularly in the neck, armpits, and groin areas, as the immune system attempts to respond to the viral invasion.
Skin manifestations frequently appear during this early stage, including unexplained rashes that may be flat or slightly raised. These rashes commonly appear on the torso, face, palms, or soles of the feet. Night sweats, headaches, and muscle aches are also prevalent during the acute infection period. Gastrointestinal symptoms such as nausea, vomiting, and diarrhea may occur, further mimicking common viral infections.
Sore throat and mouth ulcers represent additional early indicators that many people dismiss as minor ailments. The combination of these symptoms typically lasts for several days to weeks before subsiding, leading many individuals to believe they have recovered from a routine illness.
Why Early HIV Symptoms Are Frequently Overlooked
The similarity between early HIV symptoms and common viral infections creates a significant challenge for early detection. Most people experiencing flu-like symptoms naturally attribute them to seasonal illnesses, stress, or minor infections that resolve without medical intervention. This assumption often prevents individuals from seeking testing during the most critical period for early intervention.
Healthcare providers may also face diagnostic challenges, as the symptoms alone are not specific enough to immediately suggest HIV infection without additional risk factor assessment. Many individuals do not disclose potential exposure risks during routine medical visits, further complicating the diagnostic process.
The timing of symptom onset also contributes to oversight. The acute phase occurs during the window period when standard antibody tests may still show negative results, even though the virus is present and highly contagious. This creates a false sense of security for individuals who test too early after potential exposure.
Social stigma surrounding HIV continues to influence healthcare-seeking behavior, with some individuals avoiding testing due to fear of discrimination or judgment. Additionally, populations at higher risk may have limited access to healthcare services, preventing timely evaluation and testing.
How Lifestyle and Health Factors Affect Immune Function
Nutritional status plays a crucial role in immune system function and the body’s ability to respond to viral infections. Individuals with poor nutrition, particularly deficiencies in vitamins A, C, D, and E, along with minerals like zinc and selenium, may experience more severe symptoms or prolonged illness periods. Protein malnutrition specifically impacts the production of antibodies and immune cells necessary for fighting infections.
Chronic stress significantly affects immune function through the release of cortisol and other stress hormones that suppress immune responses. People experiencing ongoing psychological stress, financial hardship, or social isolation may find their bodies less capable of mounting effective immune responses to viral challenges.
Sleep deprivation consistently undermines immune function, with studies showing that individuals getting less than seven hours of sleep per night have increased susceptibility to infections and slower recovery times. Quality sleep is essential for the production and function of immune cells, including the CD4+ T cells specifically targeted by HIV.
Substance use, including alcohol consumption and recreational drug use, can impair immune function and increase vulnerability to infections. Alcohol specifically interferes with the function of immune cells and can worsen the progression of HIV infection if present.
Pre-existing health conditions such as diabetes, cardiovascular disease, or autoimmune disorders can complicate the immune response to HIV infection. These conditions may mask symptoms or create additional health challenges that overshadow potential HIV-related symptoms.
Understanding How the Body Responds to Viral Stress
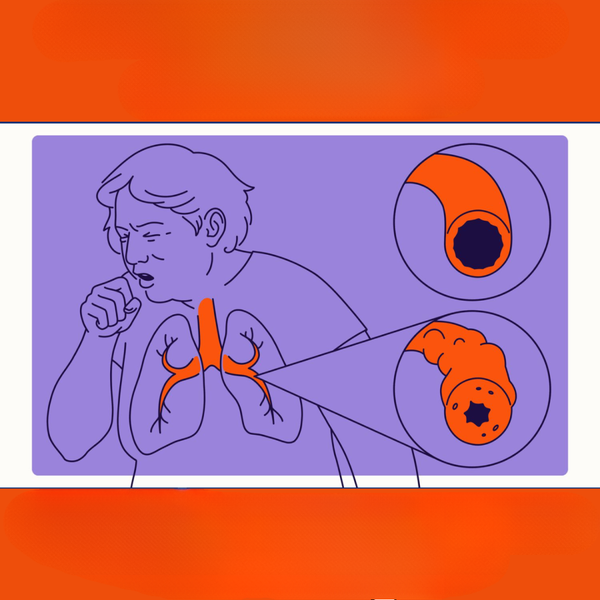
When HIV enters the body, the immune system immediately recognizes it as a foreign invader and begins mounting a defense response. This initial response involves the activation of various immune cells, including macrophages, dendritic cells, and natural killer cells, which work to contain and eliminate the virus.
The inflammatory response triggered by viral invasion leads to many of the symptoms experienced during acute infection. Cytokines, chemical messengers produced by immune cells, cause fever, fatigue, and muscle aches as the body attempts to create an environment hostile to viral replication.
As the infection progresses, the virus specifically targets CD4+ T cells, gradually depleting their numbers and compromising the immune system’s ability to coordinate effective responses. This depletion occurs slowly over months to years, often without obvious symptoms, which is why many people remain unaware of their infection status.
The body’s attempt to replace destroyed CD4+ T cells leads to increased immune system activity, which can cause chronic inflammation and contribute to long-term health complications. Understanding this process helps explain why early detection and treatment are so critical for maintaining immune function and overall health.
During the chronic phase of untreated HIV infection, the immune system becomes increasingly compromised, making individuals susceptible to opportunistic infections and certain cancers that healthy immune systems would typically prevent.
Recognizing the signs of HIV infection and understanding how the virus affects immune function empowers individuals to make informed decisions about testing and healthcare. Early detection enables prompt treatment initiation, which can preserve immune function and prevent transmission to others. Anyone who suspects potential exposure or experiences unexplained symptoms should consult healthcare providers for appropriate testing and evaluation.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




