Why New Ideas About Neuropathy Pain Relief Are Getting So Much Attention Today
Neuropathy pain is drawing growing interest as new research examines how nerve signaling, circulation and lifestyle factors influence ongoing discomfort. Fresh perspectives on symptom tracking, supportive care approaches and long-term management are shaping broader conversations about how neuropathy is understood today. These developments are creating interest in clearer information, practical strategies and emerging insights that contribute to a more informed view of nerve-related pain.
Nerve damage and chronic pain have long challenged both patients and healthcare providers. For decades, approaches to managing neuropathy focused primarily on symptom suppression rather than understanding underlying mechanisms. Today, a noticeable shift is underway as scientific inquiry deepens and clinical practices adapt to incorporate more comprehensive perspectives on nerve health and pain management.
What Are Recent Findings in Neuropathy Research Revealing?
Recent scientific investigations have expanded understanding of how peripheral nerves respond to injury and disease. Researchers are examining the role of inflammation, metabolic dysfunction, and cellular repair processes in nerve damage progression. Studies now suggest that neuropathy involves complex interactions between immune system responses and nerve cell health, rather than simple mechanical damage alone.
Advances in imaging technology allow scientists to observe nerve structure changes in real time, revealing patterns previously hidden from view. These observations have led to recognition that nerve regeneration potential varies significantly among individuals, influenced by factors including blood sugar control, nutritional status, and genetic predisposition. This growing body of evidence encourages more personalized approaches to addressing nerve-related discomfort.
Additionally, investigations into pain signal transmission have identified multiple pathways through which damaged nerves communicate distress to the brain. Understanding these pathways helps explain why identical nerve injuries produce vastly different pain experiences across patients, opening doors to more targeted intervention strategies.
How Does Tracking Symptoms and Evaluating Long-Term Patterns Improve Care?
Systematic symptom monitoring has emerged as a valuable tool in managing chronic nerve conditions. Healthcare providers increasingly encourage patients to maintain detailed records of pain intensity, triggers, and relief factors. This documentation creates a clearer picture of disease progression and treatment effectiveness over time.
Long-term pattern analysis reveals important insights that single appointments cannot capture. For instance, tracking may show that certain activities, dietary choices, or environmental factors consistently worsen or improve symptoms. Recognizing these patterns enables individuals to make informed lifestyle adjustments that complement medical interventions.
Digital health tools have made symptom tracking more accessible and precise. Mobile applications designed for chronic pain management allow users to record data quickly and generate visual reports for healthcare discussions. This technology facilitates better communication between patients and providers, ensuring treatment plans remain responsive to changing needs rather than static over months or years.
Furthermore, longitudinal data collection contributes to broader research efforts. Aggregated information from thousands of patients helps researchers identify common trajectories and potential intervention points, ultimately benefiting entire patient populations.
Why Is Public Understanding of Chronic Pain Mechanisms Changing?
Educational initiatives and increased access to medical information have transformed how people perceive chronic pain conditions. Where nerve pain was once dismissed as purely psychological or exaggerated, current understanding recognizes it as a legitimate physiological phenomenon with measurable biological markers.
Public health campaigns emphasize that chronic pain involves actual changes in nervous system function, not simply prolonged acute pain. This distinction matters because it validates patient experiences and reduces stigma that previously prevented many from seeking appropriate care. Greater awareness also encourages earlier intervention, which research suggests may prevent some irreversible nerve damage.
Media coverage of scientific advances has played a role in shifting perceptions. As mainstream outlets report on breakthrough research and novel approaches, general audiences gain exposure to concepts like neuroplasticity and central sensitization. This broader understanding fosters more productive conversations between patients and healthcare providers, as both parties share common vocabulary and conceptual frameworks.
Social support networks, both online and in-person, have amplified patient voices and shared experiences. These communities provide emotional support while also serving as information exchanges where individuals learn about management strategies and research developments.
What Are Evolving Views on Nerve-Related Conditions?
Historically, nerve damage was viewed as largely irreversible, with limited treatment options beyond symptom management. Contemporary perspectives recognize greater potential for nerve healing and adaptation than previously believed. While complete reversal remains uncommon, evidence suggests that supportive interventions can slow progression and sometimes restore partial function.
The medical community now acknowledges that neuropathy encompasses a spectrum of conditions with varied causes, from diabetes and autoimmune disorders to chemotherapy side effects and nutritional deficiencies. This recognition has led to more thorough diagnostic processes that identify underlying factors rather than treating all nerve pain identically.
Interdisciplinary care models are gaining acceptance as standard practice for complex nerve conditions. Teams that include neurologists, pain specialists, physical therapists, and nutritionists can address multiple aspects of neuropathy simultaneously, potentially achieving better outcomes than single-specialty approaches.
Patient autonomy and shared decision-making have become central to modern care philosophies. Rather than prescribing uniform protocols, healthcare providers increasingly work collaboratively with patients to develop individualized plans that align with personal values, goals, and circumstances.
How Are Emerging Perspectives on Neuropathy Pain Management Being Applied?
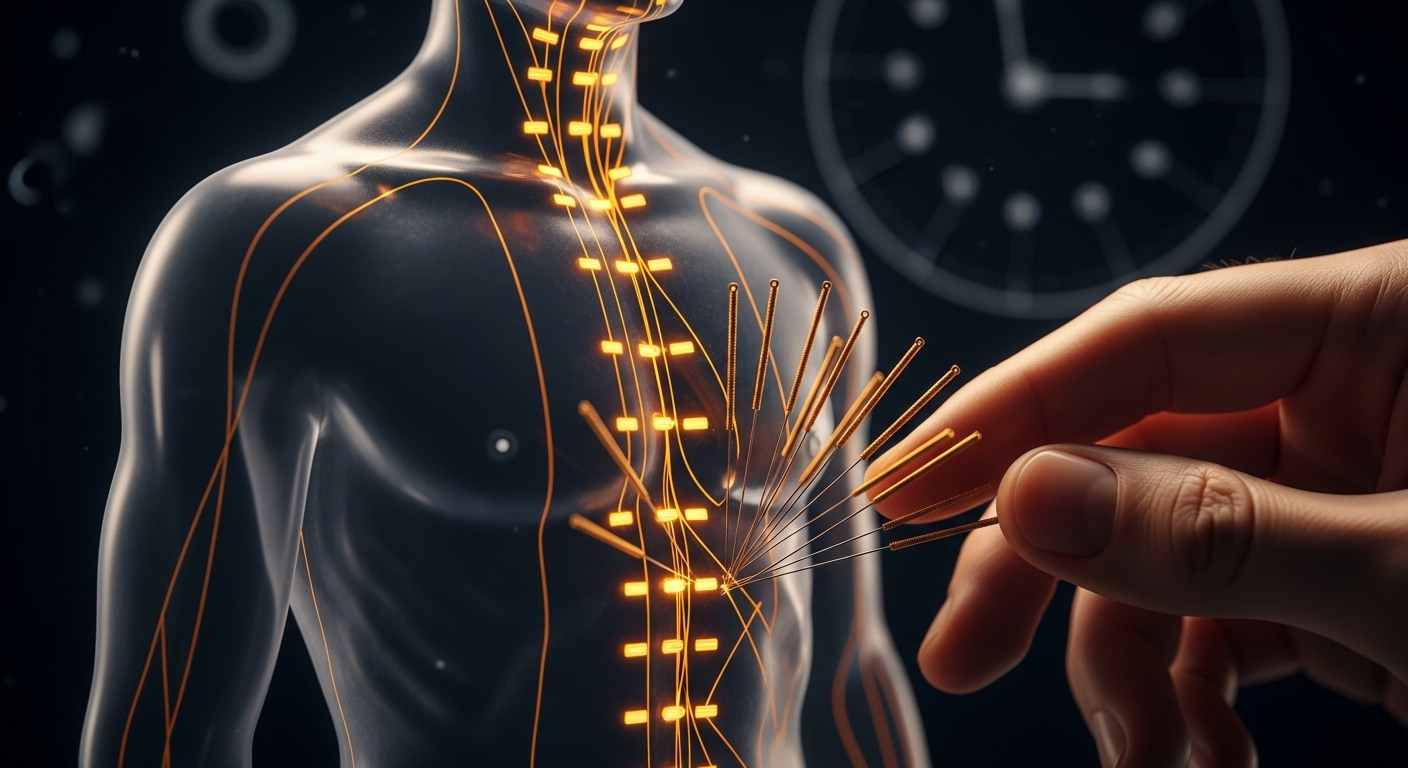
Clinical practice is incorporating research findings through updated treatment protocols that emphasize multimodal approaches. Rather than relying solely on pharmaceutical interventions, comprehensive plans may combine medication with physical therapy, lifestyle modifications, and complementary techniques.
Physical rehabilitation has gained prominence as evidence accumulates regarding exercise benefits for nerve health. Specific movements and activities can improve circulation to peripheral nerves, enhance balance, and maintain muscle strength despite sensory deficits. Therapists now design programs tailored to individual neuropathy presentations and functional limitations.
Nutritional support receives increased attention as studies link specific deficiencies to nerve damage and impaired healing. Healthcare providers routinely assess vitamin B12, folate, and other nutrient levels, recommending supplementation or dietary changes when appropriate. Blood sugar management remains critical for diabetic neuropathy, with continuous glucose monitoring technology enabling tighter control.
Psychological support is increasingly integrated into neuropathy care, recognizing that chronic pain affects mental health and that emotional wellbeing influences pain perception. Cognitive-behavioral approaches help patients develop coping strategies and maintain quality of life despite persistent symptoms.
Emerging technologies, including neuromodulation devices and advanced topical formulations, offer additional options for individuals who do not respond adequately to conventional approaches. While these innovations require further study, early results suggest promise for expanding the therapeutic toolkit available to patients and providers.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
The growing attention to new ideas about neuropathy pain relief reflects genuine progress in scientific understanding and clinical practice. As research continues and awareness expands, individuals affected by nerve-related conditions can access more sophisticated, compassionate, and effective care approaches than ever before. This evolution represents not a single breakthrough but an accumulation of insights that collectively improve outcomes and quality of life for millions navigating the challenges of chronic nerve pain.




